
How Englewood Health has united with our communities to confront a once-in-a-lifetime crisis
Voices of Englewood
When did you first realize this pandemic was unprecedented?
“This pandemic was unprecedented in ways we couldn’t imagine. We soon realized that our patients and their families needed human touch. We needed them to know they weren’t alone.”
— Lorraine Johnson, RN
Senior Coordinator of Patient and Family Engagement
“It was early in March, and I was in Maryland at a nursing conference. We had our first patient transferred to the ICU, and I believe it was the next day that we had our second patient. I got a call from work saying, ‘You need to come home.’ I knew then, this was rapidly evolving.”
— Denise Arzoomanian, RN
Senior Director of Nursing, Critical Care Services, and Professional Practice
“I distinctly remember our world changing on March 4, when patients started coming to the emergency department with fevers and respiratory symptoms. This felt much different from a traditional flu season. Being able to support my team was one of the most rewarding moments of my career. The team in our emergency department pulled together and supported each other, working tirelessly to ensure prompt care for our community. I couldn’t have done it without them!”
— Terry Bertolotti, RN
Nurse Manager, Emergency Department
When did you feel that things had turned a corner and began to improve?
“The community rallied behind Englewood Health, and many of our friends and neighbors generously provided financial support. We set up the Power to Prepare Fund to help our team have the resources and supplies to continue delivering lifesaving care.”
— Debra Albanese
Executive Vice President, Englewood Health Foundation
“Before the vaccine was made available, only basic public health measures like social distancing and masking could prevent more people from being hospitalized, and our community did everything they could to stay safe.”
— Dr. Alexandra Gottdiener
Chief of Medicine
“The moment I felt we were turning a corner was when we began giving the vaccine. Before then, even when the numbers improved, no one ever really looked relaxed; there was always a sense of anxiety.”
— Dr. Tanganyika Barnes
Internal Medicine Residency Program Director
Chapter 1
The Virus Emerges
Hospitals and first responders must be ready to expect the unexpected. But there are moments when life challenges us in ways no one can anticipate. Here’s what the Englewood Health community did in the face of such an event.
Chapter 1
The Virus Emerges
Hospitals and first responders must be ready to expect the unexpected. But there are moments when life challenges us in ways no one can anticipate. Here’s what the Englewood Health community did in the face of such an event.
The Sound of Distant Thunder
Early on, even the experts were observers, wondering what a virus emerging on the other side of the world would mean for those closer to home.
“We became aware that there was a new virus abroad, but information was sparse. It wasn’t a total shock, because we’d had two past coronavirus outbreaks, with SARS and MERS. But those never really spread worldwide. When we started to see COVID-19 cases rise in Europe, that’s when it hit home that this may be very serious.”
—Dr. Ashwin Jathavedam
Chief, Infectious Disease
“When we first heard there was a potentially novel virus, our team paid attention. And when we heard there were reports of sustained person-to-person transmission—it was a red flag.”
—Dr. Hillary Cohen
Vice President, Medical Affairs;
Chief, Emergency Medicine

“In January we established a task force to develop a comprehensive and multilayered strategy that would help to safeguard patients, staff, visitors, and the community at large. This early focus on readiness proved significant because in just a few short weeks the virus landed at our doorsteps as a real and present danger.”
— Kathleen Kaminsky, RN
Senior Vice President, Patient Care Services, Chief Nursing Officer
Setting Up the Command Center
“Typically, the command center is set up to organize the team to respond to a major disaster, like a hurricane or major incident involving mass injuries. They take over a meeting room, and there’s a bank of telephones and computers, and it’s staffed by people who can triage issues and problems and coordinate teams. But with COVID-19, we couldn’t put everybody in a room together anymore.”
—Richard Sposa
Director of Emergency Medical Services
Daily touch-bases within the organization soon morphed into standing group calls that included physician leaders from several hospitals and healthcare systems in Bergen County.
Preparing a Hospital for the Unknown
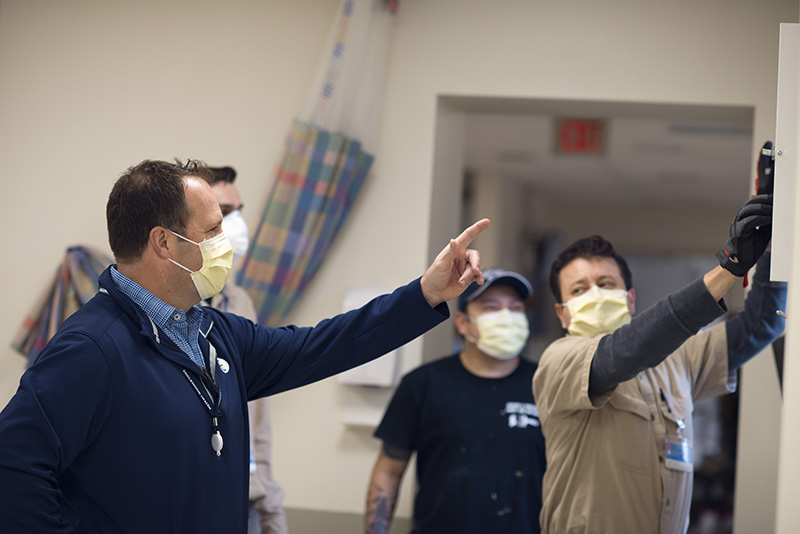
The sound of hammers and saws filled the air, making room for more critically ill patients who required ICU care and respiratory support, and clinicians worked overtime to adjust to rapidly shifting patient needs.
“Once the first wave hit, it was clear that COVID-19 spreads from droplets and masking was essential, especially with asymptomatic spread. The next step was that we had to ask everyone to mask everywhere to stay safe.”
—Melissa Capalad, RN
Infection Prevention
“My first reaction was, ‘What’s a COVID-19 test?’ Then we literally had to figure it out and bring it together within a weekend, in time for the following Monday, when we opened the testing site. We organized a new way to interact with our teams and our patients to minimize exposure, identify multiple symptoms, test safely, and quarantine quickly. This is what operations people do. You have a problem; you just figure out how to solve it.”
—Moishe B. Singer
Senior Director, Primary Care,
Englewood Health Physician Network
“You look at the heroes who don’t get mentioned—the facilities people came in and retrofitted windows in the emergency department to increase airflow and make the area safer. All of this happened overnight.”
—Dr. Hillary Cohen
Vice President, Medical Affairs; Chief, Emergency Medicine



Recognizing the Greater Good
One of the greatest contributions of local residents came not from what they did but from understanding what they shouldn’t do. Their willingness to adapt early and quickly to a strange, new existence undoubtedly saved lives and reduced stress on those caring for the sick.
“We were very grateful that people understood that public health depends on everyone working together for the collective good. By taking the appropriate precautions to protect themselves and those around them, the entire community played a role in our response to the pandemic.”
—Jamie Ketas
Vice President of Quality

The First Wave Crashes
As the virus made its way into the heavily populated Northeast, an outbreak was traced to a gathering in New York and included residents from New Jersey. With contact tracing, it soon became clear that this community was at risk of becoming a COVID-19 hotspot.
“Within a couple of days we had our first patient. Then the numbers were increasing rapidly; we were talking to each other about how we would triage people. We knew we would have to separate and quarantine people, starting in the emergency department.”
—Dr. Carmine Gianatiempo
Intensive Care Unit
“You could see the anxiety, and it was kind of painful to see that. We had to provide reassurance and let them know that the protocols work, the protective equipment works, and if they used it correctly they were going to be OK.”
—Diana Torres, RN
Infection Prevention Manager
“We knew by mid-March that we were going to be experiencing an avalanche of patients that needed hospitalization. After a couple of weeks we really started to come together as a team to solve problems and develop treatment protocols. It was an amazing group with a great sense of esprit de corps.”
—Dr. Alexandra Gottdiener
Chief of Medicine
“At the beginning, we were scared about what was happening. We were strong and supported each other. Every day is a challenge but we can conquer this.”
—Teresa Sole, RN
Staff Nurse, COVID-19 unit

“When we had that very first patient, there was a lot of fear. We created videos for staff to reinforce how to properly put on and take off your personal protective equipment. There’s a certain protocol you have to use, not to contaminate yourself when you remove it. We had patients in the ICU, and every time we went in there it was a little nerve-wracking just because no one had a sense of how infectious this new virus was. Is it like Ebola, where a drop of sweat touches you and you get infected, or is it aerosolized with coughing? At that point we had very, very little information to go on.”
— Dr. Jathavedam
Chapter 2
The Hospital Gears Up
As the virus spread, everyone at Englewood Health needed to move quickly to deliver the highest standard of care to the increasing number of patients.
Chapter 2
The Hospital Gears Up
As the virus spread, everyone at Englewood Health needed to move quickly to deliver the highest standard of care to the increasing number of patients.
A Crash Course in Everything
For years before March 2020, Englewood Health put considerable time and work into preparing for emergencies, everything from storms and power outages to active shooter situations and mass casualty events. Pandemics were no exception—the hospital had a plan in place for these as well. “A few years back, when we were preparing for H1N1 flu, we redefined our emergency preparedness policies, based on CDC and Department of Health guidelines,” says Harvey Weber, vice president for facilities management and emergency preparedness.
That policy was wide-ranging, covering support services as well as clinicians, Weber says. “We wanted to make sure our environmental services people were trained in donning and doffing PPE appropriately and understood what cleaning measures were needed to protect us from the virus,” he says.
COVID-19’s spread appeared to be unprecedented in our lifetime. Hospitals in the epicenter soon halted outpatient services and elective procedures. At Englewood Health, people from those areas were redeployed in areas that needed them. “Everyone who was going to come into contact with patients — in food and nutrition, facilities, environmental services, security — had to adapt to the quickly changing safety protocols,” Weber says.


“Everyone who was going to come into contact with patients — in food and nutrition, facilities, environmental services, security — had to adapt to the quickly changing safety protocols.”
— Harvey Weber
Vice President for Facilities Management and
Emergency Preparedness
As infection prevention manager, Diana Torres, RN, was central to much of that training. One big task was translating CDC guidance that “would change in the blink of an eye,” she says. “We collaborated with our communications team to get the word out, but we also had to go up to the clinical units and educate the people who were in direct contact with patients about changes in protocol in real time.”
Ideas about treatment also evolved quickly and constantly, says Kathleen Kaminsky, RN, senior vice president of patient care services and chief nursing officer. “We started seeing themes emerge about what worked and what didn’t,” Kaminsky says. When “proning” — turning ventilated ICU patients on their stomachs to improve oxygenation — turned out to be helpful, the Englewood team added it to their treatment protocols. But that, too, required a new initiative: to recruit and train a proning team that knew how to perform that delicate process.
Torres and most others at Englewood also had to face another issue — how to keep family members safe from a disease about which so little was known. In many cases, families had to live apart from one another to minimize any potential exposure. “That was really difficult, but it was the safest thing to do,” says Torres. She and many others tell of elaborate routines of showering and changing clothes at the end of the day before seeing their loved ones. Rick Sposa, director of EMS, notes that before the pandemic, his young daughters had loved running across the lawn to meet him when he got home and having him spin them around. “Now I couldn’t let them come near me, and they didn’t really understand,” he says.
“At a time of unparalleled uncertainty, as a surgeon, I felt a deep responsibility to stand alongside frontline workers to aid our community. Years from now when my son is learning about the COVID-19 pandemic, I can tell him I did everything I could, to the best of my ability.”
— Dr. Celinés Morales-Ribeiro
Bariatric Surgery
Transforming a Hospital
Another immediate change was to reconfigure large sections of the hospital to accommodate the influx of COVID-19 patients. Before the crisis, the hospital had 12 intensive care beds. Space for 50 additional ICU beds came in part by reconfiguring another 22-bed unit. Overnight, construction crews were drilling holes through walls and bringing in equipment, and within 72 hours the new rooms were ready.
In addition, the hospital’s engineering and construction teams had to create negative pressure rooms, designed to keep the airborne virus from reaching other parts of the hospital. That change was made all the more crucial by an evolving understanding not only of how the virus was passed along but also of what was clinically effective, Weber says.
“It was amazing to see the grit, resilience, and sheer will and determination of the team to care for our patients. Not only did our nurses care for our patients with extraordinary sensitivity, but they also cared for each other,” Kaminsky says.
“It was amazing to see the grit, resilience, and sheer will and determination of the team to care for our patients.”
— Kathleen Kaminsky, RN
Senior Vice President of Patient Care Services and Chief Nursing Officer
Learning from Peers
Another common theme cited by those who were involved in gearing up for this monumental challenge is that they couldn’t have gotten it done without collaboration from their peers at other institutions. “Early on, I started getting calls from my colleagues in other hospitals in our area,” says Weber. “We talked about what we were experiencing, what we needed, where resources were coming from.” They shared what they had, doing whatever they could to help meet immediate needs in one place with the assurance that in a few days or weeks or months, PPE, IV pumps, ventilators, and other supplies could be shifted somewhere else.
That kind of cooperation was happening among hospital systems that normally worked independently. Now they freely shared clinical knowledge. Dr. Stephen Brunnquell describes an informal consortium of clinicians from seven area hospitals and health systems who had daily calls to talk about what they were learning. “Every day, seven days a week, we would describe patients to each other and talk about what medicines we were using and what worked,” says Dr. Brunnquell.
One major result was the realization, noted by many of those on the daily calls, that blood clots in COVID-19 patients were resulting in many heart attacks and strokes. So experts across the country devised protocols in order to prevent people from clotting.
During all this, as people at the hospital looked for solutions to problems and challenges that seemed to change almost daily, many found themselves stretched beyond exhaustion, fueled only by adrenaline and caffeine. It was hard and often heartbreaking, “but we knew what we had to do to care for everyone,” says Kaminsky. “You had to do the best you could to support the team. Because this isn’t just where we worked. It’s where many of us live, and where we get our care. It’s our community.”


“How do you face a pandemic? At Englewood Health, we may not have done it holding hands, but we did join together as a team. We encouraged each other, we listened to each other, and we faced these challenges together.”
— Vicki Hoffman
Vice President, Operations
Chapter 3
A Community Rallies
Whether in support of the healthcare workers or fellow neighbors in need, Englewood and the surrounding communities united to help one another pull through this challenging time together.
Chapter 3
A Community Rallies
Whether in support of the healthcare workers or fellow neighbors in need, Englewood and the surrounding communities united to help one another pull through this challenging time together.

“I feel serving the community is ingrained in everyone at Englewood Health. That fundamental value is why I love being a part of this team. During this difficult time, we came together to help those around us however we could.”
— Anthony Figueroa
Community Affairs Specialist
Joining Forces to Help One Another
Traditional disaster relief programs were limited or rendered ineffective by the lockdown, so community leaders banded together to come up with ways to help residents in need. “Sanetta Ponton, executive director of the Metro Community Center, started holding weekly Zoom calls and inviting local nonprofits, people from faith-based organizations, town council and board of education members—just anyone who wanted to help,” recounts Janet Sharma, the coordinator of Age-Friendly Englewood, a local organization dedicated to helping Englewood’s elderly age in place. “We would identify gaps in service and talk about how to address them.”
The group collectively organized volunteers to help nonprofits like The Community Chest and the Bergen Family Center to get groceries to seniors and families sequestered at home. They also worked to bring internet access to low-income families.
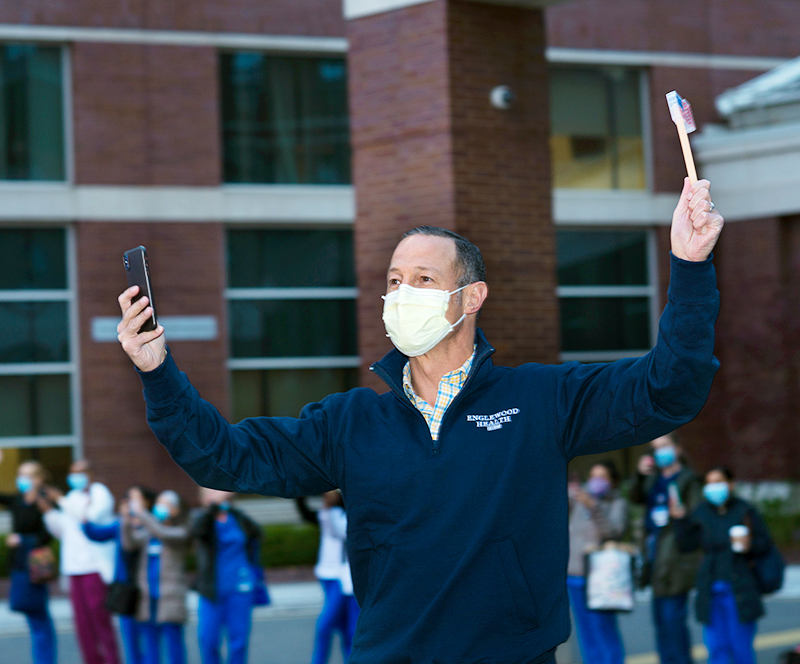
Hope came from the way people in the Englewood community stepped up. “From the very beginning, every group in our community reached out and asked how they could help,” says Warren Geller, president and CEO, Englewood Health. In many cases, support came in the form of financial contributions to the hospital foundation’s newly established Power to Prepare Fund, which raised over $4 million.
“With extraordinary strength, resilience, and generosity, our donors create an impact for countless patients at Englewood Health 365 days a year,” says Debra Albanese, executive vice president, Englewood Health Foundation. “During this especially difficult time, we are immensely grateful for the support our donors showed us. Through philanthropic donations big and small, they supported the continuity of high-quality care for all our patients, helped us obtain necessary supplies and equipment to aid in screening and treatment, and delivered much-needed support for our indispensable caregivers on the frontlines.”
Comfort Comes from Caring Neighbors
Restaurant lover Bari Adler created a plan that coupled two goals — supporting healthcare workers with meal deliveries and helping area businesses, especially restaurants, keep their doors open and their workers employed. In March of 2020, $30,000 was raised by the community to buy thousands of meals for hospital workers prepared by local restaurants. “The idea was to give thanks to them for working while the rest of us were home,” she told ABC News. Over the weeks and months to follow, more restaurants, local nonprofits, and residents stepped up to deliver meals to the hospital staff.
Those meals meant far more than sustenance. “It was amazing how we witnessed the community rally together to support local businesses and especially restaurants. In turn these restaurants fed our frontline workers thousands of meals during the toughest time of the pandemic, day in and day out,” said Nancy Bergman, director of food and nutrition.
“Two artists from the school came in to do amazing drawings, each with a different theme and inspirational message. The staff loved them.”
— Cathleen Keavey, RN
Nurse Manager, ICU
Inspiring Artwork
Other ideas to inspire and support healthcare workers originated at the hospital and were quickly embraced by people eager to help, explains Cathleen Keavey, RN, nurse manager, ICU, who describes what happened when the hospital approached the Art School at Old Church about creating inspirational whiteboards to display on each floor of the hospital.
“Two artists from the school — Sarah Smith and Donna Dolby — worked with dry erase markers to create amazing displays, each with a different theme, and wrote inspirational messages that reminded nurses that many patients were going home to their families because of them,” says Keavey. “The artists told us they were so happy to come and do something to show the nurses that the community was grateful for their care, and the staff loved them. They brought in some sunshine.”
Also uplifting were students — some as young as kindergartners — who created art, music, and messages organized by their teachers and sent to the hospital over the months to follow. “Their colorful and heartfelt messages on display at nursing stations and throughout the hospital reminded the hospital staff that superheroes were real,” says Barbara Grygotis, RN, senior director, medical/surgical and nursing operations.

Recognition from First Responders
One of the most memorable demonstrations of gratitude and support came at dusk on April 24, when the Englewood Fire Department led a parade of fire, police, and emergency service vehicles around the hospital campus. First responders from more than a dozen Bergen County communities participated, blasting their sirens, flashing their lights, and waving and cheering to the healthcare workers gathered outside and those watching from hospital windows.
The acknowledgment of the work being done at the hospital by first responders sent a powerful message, said Warren Geller, president and CEO, Englewood Health, speaking after the event. “Men and women who put their lives on the line for us came out to honor us,” he said. “I’m speechless. This is what we do. We exist to be here for our community. To be recognized by these folks — what an honor. What a great night,” said Dr. Stephen Brunnquell.
The parade also served as a visual — and audible — reminder of what the entire community of Englewood had been able to achieve. “Coming together during a time when we were all separated from each other showed our tremendous resilience as a community and how connected we truly are,” says Geller.
“Tonight was about letting everyone at Englewood Health know that we are behind them and we are proud of them and everything they are doing to treat the patients suffering from COVID-19 and everything they are doing on the frontlines.”
— Jeff Kaplan
Captain, Englewood Fire Department


A Song of Hope
Local musicians George Bosotina and Emily Herring wrote a song for Englewood Health during COVID-19. “For two people in music feeling unable to do anything to make difference, it was a way to give back,” explains Bosotina. “It gave us the chance to use something that we know how to do to help the healthcare teams who were out there every day.”
The song “It Only Gets Better” came to them quickly, fueled by their experience of those early pandemic days. “It was that period in late March 2020 when everyone felt confused, depressed, isolated, and scared, and the song reflected what we were seeing and feeling at the time,” says Herring. “But we also knew there had to be hope, so we wrote about making it through this together.”
Their music and lyrics’ message of resiliency resonated with the hospital staff and community members.
“It Only Gets Better” was released in a special presentation to staff in April 2020, at the height of COVID-19 cases at Englewood. Bosotina and Herring also performed the song live during the Englewood Health COVID-19 Remembrance event in October 2020. In early 2021, it also became the soundtrack of a public service announcement encouraging the community to get vaccinated, jointly performed by students from the Performing Arts School at BergenPAC.
“The act of doing this and it taking on a life of its own gave us a positive experience at a time of a lot of negativity,” says Bosotina. “And it’s so wonderful that the song we wrote was heard by so many and was about something so meaningful.”
Englewood Health and BergenPAC teamed up for a special performance of “It Only Gets Better.”

“It only gets better, when we stand together.
To tough through and get by,
Even though it’s harder than ever.
We’re gonna make it, long as we don’t break it.
Just do right, there’s no sides,
We must know it’s part of forever.”
Lyrics from “It Only Gets Better,”
by George Anthony Bosotina and Emily Eileen Herring
Chapter 4
Finding Hope
As the pandemic surged, the Englewood Health team did what was needed to keep fighting and find moments to celebrate, remember, and support each other.
Chapter 4
Finding Hope
As the pandemic surged, the Englewood Health team did what was needed to keep fighting and find moments to celebrate, remember, and support each other.
“This is What We Do”
In April 2020, Dr. Stephen Brunnquell did an interview with Steve Inskeep for Morning Edition on NPR. Unlike the dozens of television appearances he’d done to talk about being on the frontlines of the COVID-19 response, which were taped and edited down to 20-second clips, this was done live. “At one point he heard something in my voice, and he commented on it. And he was right, and it almost took my breath away. I was so proud of what we were doing at Englewood because it involved everyone. What the nurses had to do was incredible. And the surgeons pitching in, and people making phone calls, and the support coming from the community. It was all of that, and the host heard it in my voice. All of us, working together, sustained each other.”
But Dr. Brunnquell also notes that as extraordinary as the events of the past year and a half have been, and as unsparing as Englewood’s response was and continues to be, in another sense, this has been a kind of caring as usual. “My whole career has been about getting ready for this. It’s what we do. We take care of people. We never thought we’d see something like this, but this is what I signed up for,” says Dr. Brunnquell. “It was painful, but we didn’t walk away. We didn’t flinch. This is what we do.”


“My whole career has been about getting ready for this. It’s what we do. We take care of people. We never thought we’d see something like this, but this is what I signed up for.”
— Dr. Stephen Brunnquell

Caring for the Whole Person
One of the most difficult challenges for patients with COVID-19 was the lengthy isolation and separation from family and friends. Finding ways to support patients beyond clinical care “became a crucial part of helping them recover,” says Lorraine Johnson, RN, senior coordinator of patient and family engagement. “We realized that patients and their families needed human contact, if not in person, then virtually,” says Johnson. The team committed themselves to making contact with every patient, every day. “We wanted them to know they weren’t alone.”
Existing phones were replaced with ones that after a few rings would pick up automatically and switch to intercom mode, so that even the sickest patients could hear a human voice calling to check on them. “Even if the patient didn’t have the strength to lift their hand to pick up the receiver, my voice would be in the room,” says Johnson. “And it would be magic. And I would be able to say, ‘You sound clearer. You sound much better today.’ ”
The team also created a concierge service to bring patients whatever they might need, from cell phone chargers to clothes to wear when they were finally sent home. If a patient wanted something different to eat or a social worker to talk to, it would be taken care of. Staff redeployed from other departments became the lifeline for patients and their families to stay connected. The COVID-19 team served as an extension of the ICU team now caring for a majority of hospitalized patients. Oncologists, cardiologists, and surgeons stepped in to provide medical updates for families allowing intensivists and hospitalists to focus on caring for the most critically ill. “Providers whose practices were sidelined by the pandemic helped treatment teams however they could and were just incredible. ‘Where do you need me? Where can I add the most value?’ ” says Dr. Alexandra Gottdiener, chief of medicine. “They inspired us all with their willingness to pitch in and help.”
Another effort spearheaded by the patient relations team sought to fill in personal details about patients, many of whom were ventilated and couldn’t speak. “ ‘Tell me about your loved one,’ we would ask families,” Johnson says. “ ‘What are they like? Do they have a nickname? What’s their favorite thing to eat? What do they like to watch on TV? What can you give us so that when they wake up, it will make them smile?’ Families sent us pictures, of the dog and the house on the lake and the wedding.” The photos were made into a collage, laminated, and put on the door of the patient’s room “so that when someone went into that room, they’d know who those patients were and could connect with them on a human level,” she says.



“Emergency care was still needed and provided, so we pulled together whatever we needed to make sure all patients were taken care of, not just COVID-19 patients.”
— Helene Wolk
Senior Vice President, Chief Operating Officer
Offering Support When and Where it was Needed Most
As COVID-19 surged, programs to support nutritional, physical, and emotional health — in the hospital and in the surrounding community — immediately had to become virtual, says Lauren Menkes, LMSW, MPH, director of social work.
“We conducted live virtual community meetings about stress and anxiety and about parenting during the pandemic,” she says. There were also youth and adult yoga, art therapy, and a meditation series for those who were homebound. The hospital team worked with community partners. “They helped us know where the needs were, where people were struggling and needed more support,” Menkes says. “Those partnerships helped us provide the comfort and hope needed during the day-to-day uncertainty we were all living through.”
Menkes and the team also called patients and families. She remembers the family of a man in his 90s. “They knew that I wouldn’t always have a medical update,” she says. “But they would put me on speakerphone and gather the whole family together, just to talk and share experiences. It was the most loving, kind family, and they said that just being able to talk to someone who might know a little more than they did was extremely helpful and gave them hope.”
In the fall of 2020, COVID-19 numbers rose again, and so did levels of stress and anxiety inside the hospital. “We engaged departments from across the organization to ensure that team members had access to behavioral health experts and programs,” says Pat Wilson, senior vice president and chief human resources officer. “The well-being of our team remained a priority, and providing appropriate resources that matched those needs was critical,” she says.
“The well-being of our team remained a priority, and providing appropriate resources that matched those needs was critical.”
— Pat Wilson
Senior Vice President and Chief Human Resources Officer
Recognizing Disparities
“We saw firsthand how economic and racial disparities played out inside and outside the hospital,” says Eva Matos-Botex, director of talent acquisition, organizational development, and diversity in Human Resources. To address those issues both immediately and in the longer term, Englewood formed the Diversity and Inclusion Education Council, made up of 12 team members from the organization. “Our major focus is reducing healthcare disparities in the communities we serve,” says Matos-Botex, who was tapped to lead the new group.
The council also created an educational program to address diversity in the workplace. “We want to make sure that everyone understands not just our differences but also what our similarities are,” says Matos-Botex. The goal, she adds, is to recognize where in the workplace and in the community unconscious biases may be and to mitigate them so that they don’t impede “our ability to provide the best care, to respect the people we work with and those we’re providing care to.” To reinforce that commitment, Warren Geller joined more than 1,600 CEOs around the country to sign the CEO Action for Diversity and Inclusion pledge to help continue on the path to diminishing healthcare disparities.
Diversity and Inclusion Education Council









“From the very beginning, every group in our community reached out and asked how they could help.”
— Warren Geller
President and CEO Englewood Health
Inspiring Others
In late 2020, Englewood Health was the only hospital in the nation to receive the Leapfrog Pandemic Hero of the Year Award by The Leapfrog Group. This prestigious national honor recognized Englewood Health’s extraordinary commitment to patient safety and ensuring the health and well-being of their employees throughout the COVID-19 crisis.
“At Englewood Health, we absolutely know what it means to go above and beyond,” said Warren Geller. “Our entire team did not hesitate for one moment to care for the many communities we serve. What I witnessed—not surprisingly—was each and every member of the Englewood Health team stepping up in every way imaginable. They put everything else aside. They saved many lives. And our job as leaders was to support them every step of the way. I thank Leapfrog for recognizing this team and I am confident that we will continue to live up to this recognition in the days and months ahead.”
“We were most impressed by the people of Englewood Health, who came together in so many ways showing courage and compassion in the face of the COVID-19 crisis. They have inspired us all,” said Leah Binder, president and CEO of The Leapfrog Group.
Geller and the Englewood community also found hope in a remembrance celebration held outside the emergency department. “We released butterflies to honor those we had lost and to celebrate life going forward,” Geller says. “We remember those we knew and loved, and we continue to do what we do in their memory.”



“We remember those we knew and loved, and we continue to do what we do in their memory.”
— Warren Geller
Chapter 5
Our Future Together
The emergence of a vaccine offers light and hope to the Englewood community.
Chapter 5
Our Future Together
The emergence of a vaccine offers light and hope to the Englewood community.
A New Beginning
“Everybody was so happy to get it. People were so grateful, thanking us, taking selfies, and asking us to take pictures of them,” Brigley says. “It was such a proud moment to be a nurse. I was proud and humbled to be part of such a thing—the beginning of the end of this pandemic. In all of my career, in 40 years, I had never experienced something so big.”

Reaching the Community
The challenge is education and access — teaching about the vaccine, overcoming hesitancy, and encouraging people to get the shot. “The biggest concern was how are we going to get the vaccine to the most vulnerable parts of our population,” says GaEun Joung, pharmacy director.
Connecting directly to “the 90-year-old who didn’t even own a computer,” Dr. Brunnquell says, helped prevent many people from falling through the cracks.
The hospital organized additional vaccine events to help ensure that as many people as possible received potentially lifesaving doses. The team worked with religious leaders in communities of color to help overcome understandable and historical reluctance to receiving vaccinations. “We spoke with local religious leaders and listened very carefully to the concerns of many who were hesitant to receive the vaccine,” says Dr. Brunnquell. “We held virtual town hall meetings. We invited community groups to a dialogue to reduce anxiety and fear of the vaccines and their history. We came together to provide access to the highest levels of experts in the scientific community to answer their questions and to confront doubt and fear head on.”
“It was such a proud moment to be a nurse. I was proud and humbled to be part of such a thing — the beginning of the end of this pandemic.”
— Pat Brigley, RN
Director, Employee Health Service

“The biggest concern was how are we going to get the vaccine to the most vulnerable parts of our population.”
— GaEun Joung
Pharmacy Director
One vaccine event in downtown Englewood resulted in some 90 percent of a single senior housing development being vaccinated, Dr. Brunnquell recalls. The hospital also reached out to undocumented residents, promising to vaccinate while protecting identities. “We saw those who were coming to the vaccination clinics, and then the people who were not coming because they had concerns about the vaccine,” says GaEun Joung.
Preparing for the Road Ahead
When the next historic challenge arrives, whether borne by virus or something else, the healthcare team at Englewood Health will feel that much more prepared to serve the community. “We should always seek to learn from every experience,” Hoffman says. “We all want to be innovative on our own timeline,” she adds. “This was a reminder that sometimes innovation doesn’t come on our timeline.”
The pandemic called on workers to tap reserves of strength they may not have known they possessed. It also required the strength to admit one’s vulnerabilities. “This has taught me to rely on others, not just for the work that needs to be done, but for emotional support,” says Victoria Lange, senior director of operations and physician integration for the Englewood Health Physician Network.
Healthcare workers leaned on one another, and on social workers made available throughout the crisis. “We needed to talk to people about things. You don’t know what someone else is going through or if they had lost a loved one,” Lange says. “It was OK to be scared, and mad. And as long as you talked to people about it and didn’t try to hold that in, it was fine. A lot of people here felt comfortable with being open, and I think that’s the way to get through anything.”
Despite all the uncertainties and moments of true despair, the experience for many at Englewood Health underscored why they do what they do. Says Hoffman: “When you work in healthcare, you’re there because you care about people. You expect that when you’re called upon, you’re going to serve.”




“I have never been so proud to be a member of this team of the nurses, the doctors, and all the supporting folks at Englewood. The energy and devotion has never been so evident. We continue to care for the sick and the dying. We continue to heal as best we can. We continue to comfort and inspire patients and their families. We are able to do this because deep down all of us are people of hope.”
— Dr. Stephen Brunnquell
President, Englewood Health Physician Network
Is there a specific person or moment that stays with you — a memory you carry from this time?
“One in particular who I think about was a member of our team who was known to everyone, and when he left the hospital to go home, people lined the hallways, played music, brought him balloons. He literally got cheered and danced out of the hospital.”
— Dr. Peter Shin
“Working together with the team at Englewood Health, our students were featured in a powerful music video about the COVID-19 vaccine that they will remember forever. Their voices were heard, and it is because of Englewood Health’s commitment to our community that we can all feel safer.”
— Alexander Diaz
Director of Education and Outreach, BergenPAC
“My unit’s first COVID-19 patient admission: There was a sense of fear of the unknown. But my team came together at that moment. This marked the beginning of our COVID-19 journey, and along the way my team became the COVID-19 experts, they became the pioneers. It was all hands on deck, every role was important, every role mattered. There were a lot of tears, a lot of sweat, moments of feeling helpless, but my team fought on. We must never forget their selfless acts of heroism.”
— Omicel F. Catambay, RN
Nurse Manager
“We gathered everyone outside. It was the first time in a long time seeing all of us together. I will never forget when Dr. Brunnquell spoke and mentioned a verse from Psalm 30: ‘After the darkness and sadness of night, joy comes in the morning. May I speak for all of us when I say, Dear God, morning cannot come soon enough.’ That said it all.”
— Shanel Bailey
Security
“We had an event outside in the fall, where we gathered and released butterflies in remembrance of those who had been lost. It was very heartwarming to see so many people touched by loss all come together. But to see everyone gathered as a community also made me realize that an incredible bond had been formed. This is a memory of this time in our lives that will stay with me for a very long time.”
— Anthony Orlando
Senior Vice President, Chief Financial Officer
“I’m amazed by each and every one of you. You didn’t hesitate, even for one moment. You put aside everything else going on in your personal lives to care for others, to save others. To put an iPad in front of people so they could talk to their loved ones. To give them a squeeze on the arm because no one else was allowed in their rooms. To go so far above and beyond. I’m in awe of all of you and I couldn’t be prouder to be on your team. It doesn’t matter what your specific role is here. We’re all in the business of patient care. My heart goes out to all of you as true heroes.”
— Warren Geller
President and CEO





“I have always said that Englewood Health provides our community with access to world-class, academic-level heathcare in a compassionate, community setting. The importance of both was made evident by the pandemic. I truly could not be more proud to represent this organization, and this community who stepped up, reached out, and worked together during the last year and a half. I am especially proud of how Englewood Health has prioritized not just treating illness but keeping this community healthy.”
— Richard Lerner
Chairman, Board of Trustees




















